Mental health, which refers to “a state of well-being that enables people to cope with the stresses of life, to realise their abilities, to learn well and work well and to contribute to their communities,” is an integral part of general health and well-being and a basic human right (WHO 2022: 8). Unfortunately, this state of well-being remains elusive for millions and millions of people in India and elsewhere globally. An estimated 14.8% of India’s population experienced a mental disorder in 2021, which implies that every seventh individual was affected by a mental disorder of varying intensity (Global Burden of Disease Collaborative Network 2022).
The health, social, and economic consequences of mental health conditions are enormous. Studies suggest that people with severe mental health conditions die 10 to 20 years earlier than the general population (Chesney et al. 2014: 153). In India, it is estimated that mental disorders caused 1,971 disability-adjusted life years (DALYs) per 100,000 population, accounting for 5.25% of the total DALYs in 2021, up from 2.75% of the total DALYs in 1990 (Global Burden of Disease Collaborative Network 2022). It has been projected that mental health conditions will cost the Indian economy about US$1.03 trillion between 2012 and 2030 (Bloom 2014: 22).
The National Mental Health Survey found that 7% of adolescents aged 13-17 experienced a mental disorder in 2015-16 and that 8 to 11 million adolescents required mental healthcare at any given point of time in the country.
Adolescence is a developmentally sensitive time for a person’s mental health, characterised by both vulnerability and opportunity. Roughly half of the mental disorders amongst adults start by the mid‐teens, and three‐fourths by the mid‐20s (Kessler et al. 2007: 359), which highlights the critical importance of investing in adolescents’ mental health. Drawing on the available literature, this article focusses on mental health challenges faced by adolescents in India, which has the world’s largest adolescent population. Specifically, it discusses what is known about the prevalence of mental disorders in adolescents and how experiences during transition to adulthood affect adolescents’ mental health in India.
Prevalence of mental disorders
Although mental health research has increased, data on mental health conditions in adolescents remain limited and incomplete in India. Moreover, mental disorders are conceptualised and measured in different ways across studies. Therefore, estimates discussed in this article need to be interpreted with caution.
The available evidence indicates that notable proportions of adolescents experienced mental disorders in India. The National Mental Health Survey found that 7% of adolescents aged 13 to 17 experienced a mental disorder in 2015–16 and that an estimated 8 to 11 million adolescents required mental healthcare at any given point of time in the country (Gururaj et al. 2016: 112). A state-representative longitudinal study of more than 20,000 adolescent boys and girls in Bihar and Uttar Pradesh conducted by the Population Council (hereafter referred to as the UDAYA study) reported that 2% of unmarried boys and 5% to 8% of unmarried and married girls aged 15 to 19 displayed symptoms of moderate to severe depression during the two weeks prior to the interview in 2015-16 (Population Council 2017).
The study also found that 2% of boys and 4% to 8% of girls contemplated committing suicide in the last 12 months. According to the National Crimes Record Bureau, 6% of suicides reported in 2022 were committed by adolescents aged below 18 years (2023: 204). The 2021 Global Burden of Disease Study estimated that 14% of adolescents aged 10 to 19 – 13.4% of boys and 13.9% of girls – experienced a mental disorder in India (Global Burden of Disease Collaborative Network 2022).
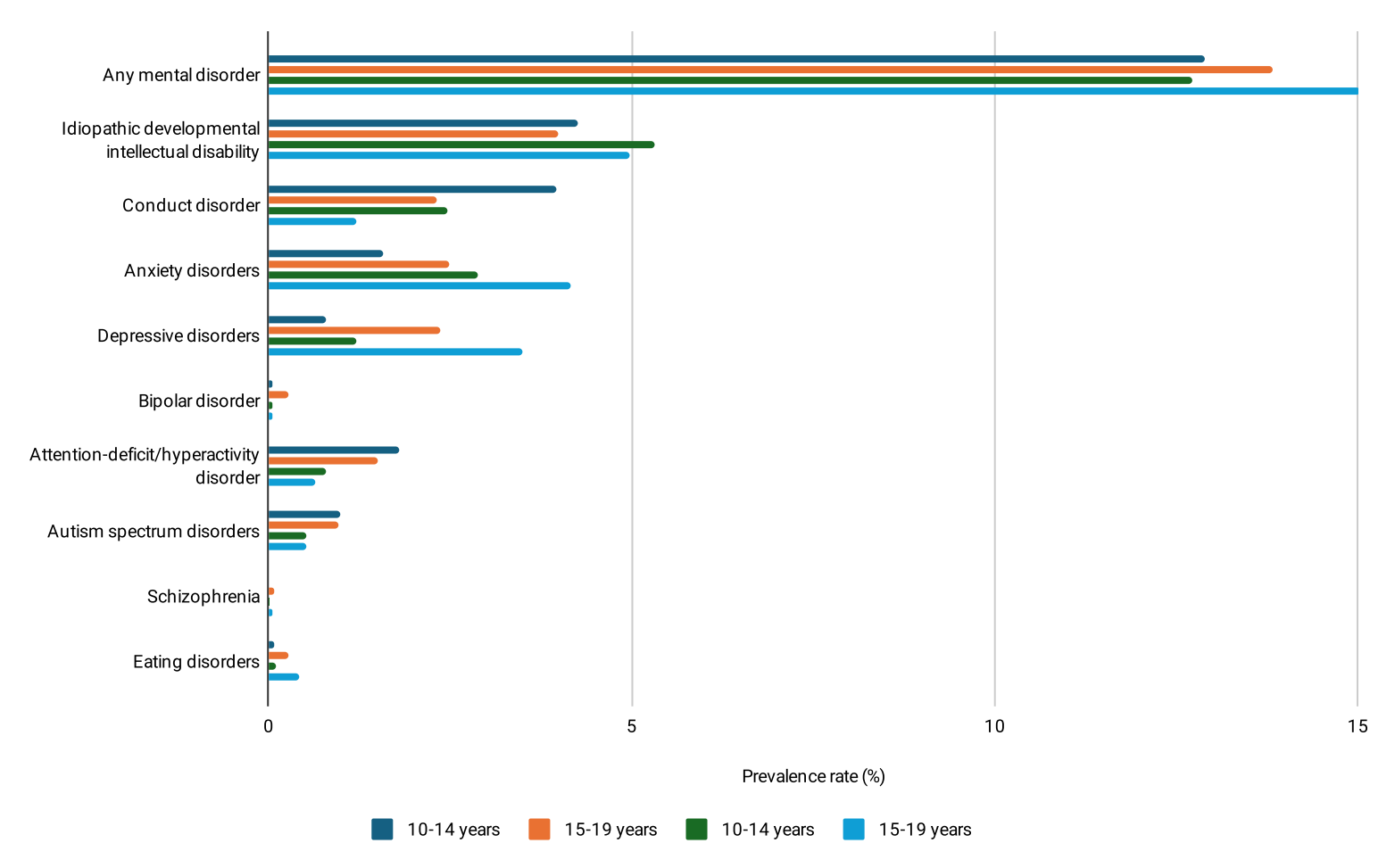
Prevalence estimates by the Global Disease Burden Initiative showed that idiopathic developmental intellectual disability – a condition of below-average intelligence or mental ability – was the most common type of mental disorder in adolescents, affecting one in 25 boys and one in 20 girls in India (Figure 1). Conduct disorder, anxiety disorders, and depressive disorders were also common in adolescents, although the prevalence of these varied by the age and sex of adolescents.
Conduct disorder was more common amongst boys, especially amongst younger boys (for example, 4.0% in boys aged 10 to 14 compared with 2.5% in girls in the same age group), while anxiety disorders were more common amongst girls, even more so amongst older girls (4.2% in girls aged 15 to 19 compared with 2.5% in boys in the same age group). Depressive disorders were more common amongst older boys and girls, more so amongst girls.
Figure 1: Prevalence of Mental Disorders in Adolescents in India
Although mental disorders in adolescents occurred in both rural and urban areas and in all states, there were some disparities. The National Mental Health Survey reported that the prevalence of mental disorders was twice as high in urban metro areas as in rural areas (13.5% versus 6.9%). According to the 2021 Global Burden of Disease Study, the prevalence of mental disorders in adolescents aged 10 to 19 ranged from 10.5% in Goa to 16.1% in Manipur.
The 2021 Global Burden of Disease Study reported that mental disorders have jumped up in the ranking of top causes of health loss in adolescents aged 10 to 19 since 1990 in India – to first place from seventh.
The state-level difference was even wider amongst girls aged 15 to 19 years—19.1% of girls experienced a mental disorder in Manipur compared with 11.8% in Goa. There were state-level variations in the prevalence of specific conditions as well. The prevalence of idiopathic developmental intellectual disability was the highest in Bihar (5.64% in boys and 6.87% in girls), for anxiety disorders, it was Manipur (3.14% in boys and 5.74% in girls), and for depressive disorders, Tamil Nadu (2.25% in boys and 3.67% in girls).
The prevalence of mental disorders in adolescents and their contribution to health loss are on the rise. The 2021 Global Burden of Disease Study reported that mental disorders have jumped up in the ranking of top causes of health loss in adolescents aged 10 to 19 since 1990 in India – to first place from seventh. And the share of mental disorders in the total DALYs in adolescents doubled between 1990 and 2021,to 12.96% in 2021 from 6.82% in 1990.
The Population Council’s UDAYA study reported that the prevalence of mental disorders, as measured by the experience of symptoms of moderate to severe depression and suicidal ideation, increased over time, and the increase was higher for girls than boys. It was the highest for married girls (Table 1). For example, the proportion of married girls who reported symptoms of moderate to severe depression in the last two weeks doubled in Bihar between 2015-16 and 2018-19 (7% versus 15%).
Table 1: Prevalence of Symptoms of Moderate to Severe Depression and Suicidal Ideation in Adolescents, Bihar and Uttar Pradesh, 2015-16 and 2018-19
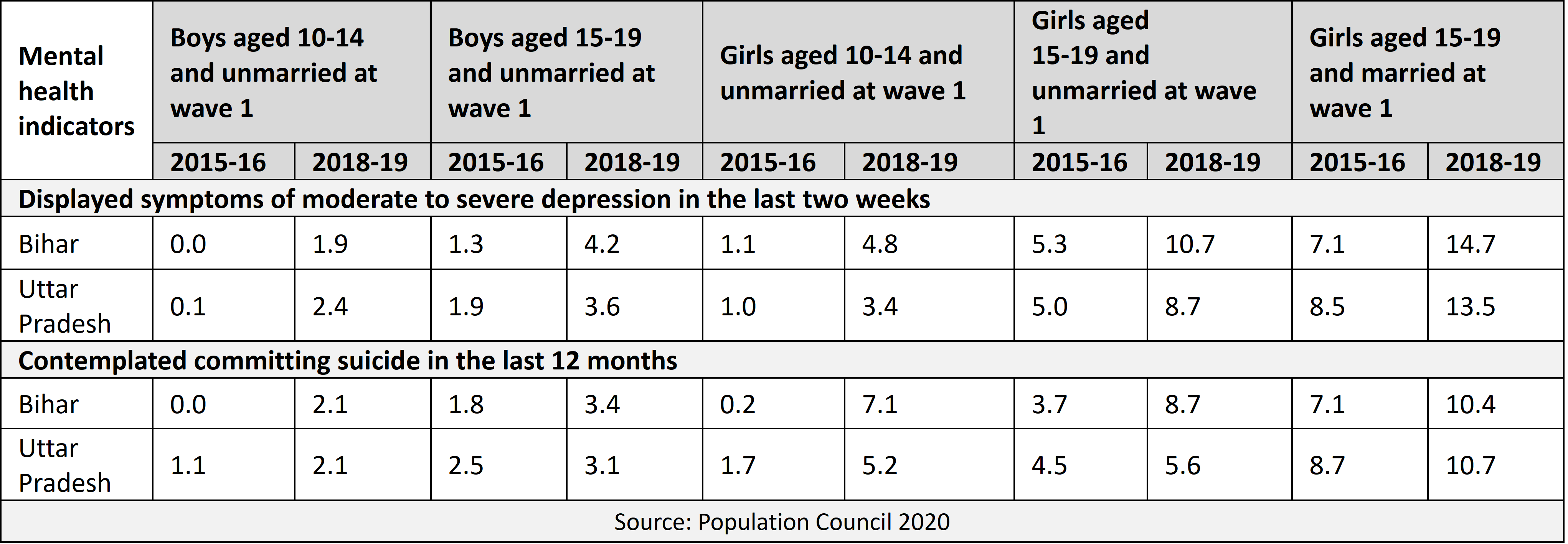
The Covid-19 pandemic increased the burden of mental disorders. Globally, it is estimated that depressive disorders and anxiety disorders increased by 28% due to the pandemic (Global Burden of Disease Collaborative Network 2022). A follow-up survey among a sub-sample of the Population Council’s UDAYA study reported that the proportion of adolescents who experienced symptoms of depression in the last two weeks increased from 34% in 2018-19 to 42% in 2020.
The 2022 World Mental Health Report notes that the approach to mental healthcare remains very much business as usual and that too many people living with mental health conditions are not getting the care they need and deserve all over the world. This is true in India too. The National Mental Health Survey reported a treatment gap of 83% for any mental health problem in the adult population in India (Gururaj et al 2016: 122). The Population Council’s UDAYA study reported that although the majority of adolescents who reported mental health conditions sought help, they, particularly girls, sought help mostly from a family member and rarely from healthcare providers. For example, of the adolescents who experienced moderate to severe depression-related symptoms in Uttar Pradesh, 64% of unmarried boys and 67% to75% of unmarried and married girls sought help. However, just 10% of boys and just 3% to 4%of girls sought help from healthcare providers.
Transition to Adulthood
The health and development situation of today’s adolescents is better than that of earlier generations in India. Even so, the transition to adulthood is marked by a premature exit from school, early entry to the labour force, early marriage, and early parenthood for many. These adverse experiences are a threat to adolescents’ mental health.
Premature exit from school
According to Unified District Information System for Education (UDISE) data for the academic year 2021-22, although nearly all students in India transitioned from primary to upper primary education (transition rate of 93% from class 5 to class 6), there was a steady decline as students moved from upper primary to secondary education (transition rate of 89% from class 8 to class 9) and from secondary to higher secondary education (transition rate of 78% from class 10 to class 11). Discontinuation from school can increase the risk of mental health conditions, although these conditions can be a risk factor for discontinuing school as well.
The chances of experiencing depressive symptoms were 0.27 times and 0.35 times lower, respectively, in boys and girls who were not engaged in paid work compared with those who were so engaged.
The Population Council’s UDAYA study reported that 25% to 27% of boys and 25% to 33% of girls who experienced symptoms of moderate to severe depression in the last two weeks reported reasons such as discontinuation of studies, fear of failure, and examination-related anxiety for feeling depressed. And further analysis of UDAYA data found that girls who were enrolled in school or any other educational courses had 40% to 60% lower chances of experiencing depressive disorder (Dhara et al. 2024: 20-24).
Early entry to labour force
While overall trends in child work and child labour have declined in India, many forms of child work and child labour continue to persist. For example, an analysis of the 2019 India Time Use Survey found that 7.5% of children aged 6 to 17 years were in child labour in 2019 (Kim and Olsen 2023: 199).
Further analysis of UDAYA data found that transitioning to paid work in childhood and adolescence increased the risk of mental health conditions, more so among girls. The chances of experiencing depressive symptoms were 0.27 times and 0.35 times lower, respectively, in boys and girls who were not engaged in paid work compared with those who were so engaged (Ganguly et al. 2023: 1137-70). Further, the risk of experiencing mental health conditions was higher for adolescents who combined schooling and paid work among both boys and girls.
Early marriage and motherhood
Although the prevalence of child marriage has declined by half over the course of this century, one in eight adolescent girls aged 15 to 19 were ever married as recently as in 2019-21 and almost a quarter of all women aged 20 to 24 were married by age 18, which means that roughly 14 million young women were married as children.
UDAYA findings highlight that marriage in adolescence is a risk factor for moderate to severe depression. The odds of reporting depressive symptoms were two times higher for unmarried girls who got married in the inter-survey period compared with those who remained unmarried (Agarwal et al. 2023). Moreover, married girls who experienced marital abuse had a higher chance of reporting depressive symptoms, more so girls who had not given birth.
Conclusions
In short, mental health conditions in adolescents are a major public health issue in India. The prevalence of mental disorders and health loss due to them in adolescents has increased. Very few adolescents with mental health conditions receive help from the health sector. Adverse experiences such as a premature exit from school, early entry to the labour force, early marriage, and early parenthood during the course of transition to adulthood adversely affect adolescents’ mental health, more so of girls.
Promoting the mental health of adolescents need actions beyond the health sector, including ensuring that adolescents live, study, work, and socialise in supportive, healthy, and safe environments that promote and protect their mental health.
India has articulated its commitment to strategically address mental health conditions in adolescents through various policies and programmes, including the National Mental Health Policy 2014, the National Health Policy 2017, the National Mental Health Programme, and the Rashtriya Kishor Swasthya Karyakram. It is important that policy prescriptions are translated into effective measures to promote adolescent mental health. Efforts are required to ensure that mental health services offered under the National Mental Health Programme and the Comprehensive Primary Health Care services under Ayushman Bharat’s Health and Wellness Centre Scheme reach adolescents, particularly vulnerable ones. Regular screening for mental health conditions in school and community settings would help early diagnosis, treatment, and support.
Promoting the mental health of adolescents needs actions beyond the health sector, including ensuring that adolescents live, study, work, and socialise in supportive, healthy, and safe environments that promote and protect their mental health. Fostering a positive and supportive school climate has the potential to improve adolescent mental health. School-based social and emotional learning programmes are found to be effective in promoting mental health, and investments are required to adapt and upscale such programmes.
Efforts to reduce children’s initiation into the labour force when they should be in school are also needed. Interventions are also required to inform and empower girls to delay the age of marriage and childbearing. These have to be in combination with interventions to influence family and community norms. At the same time, special efforts have to be made by service providers to offer married adolescent girls support and referrals for violence prevention and mitigation, pregnancy loss, or infertility.
K.G. Santhya is an economist and demographer who has conducted studies on rights of youth, gender equity, women’s empowerment, reproductive health, and gender-based violence.









