The Covid-19 pandemic resulted in the tragic loss of lives and gave rise to serious health and socio-economic crises, which amplified existing inequalities and injustices. The pandemic and the lockdowns imposed in 2020 and 2021 to control its spread had far-reaching consequences on people’s well-being.
A Covid-19 livelihoods survey by Azim Premji University in 2021 reported that eight out of 10 people in India ate less food during the pandemic than before it. Food insecurity was higher for certain groups of people, such as Muslims, Dalits, women and those with lower levels of education. There were also reports of an increase in the burden of domestic work for women and intimate partner violence on women.
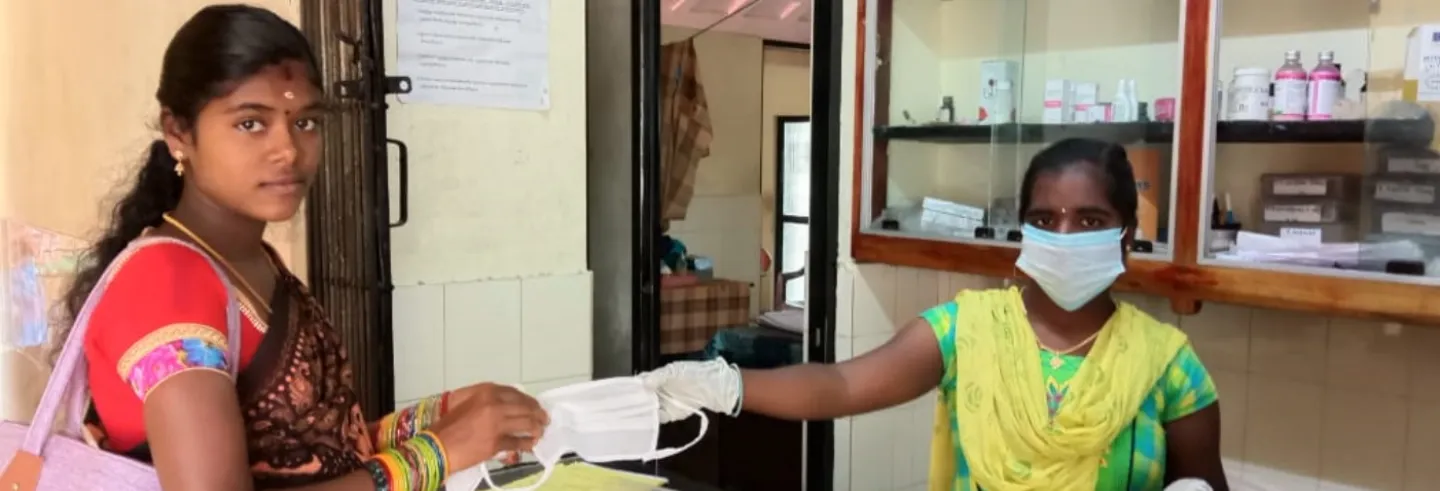
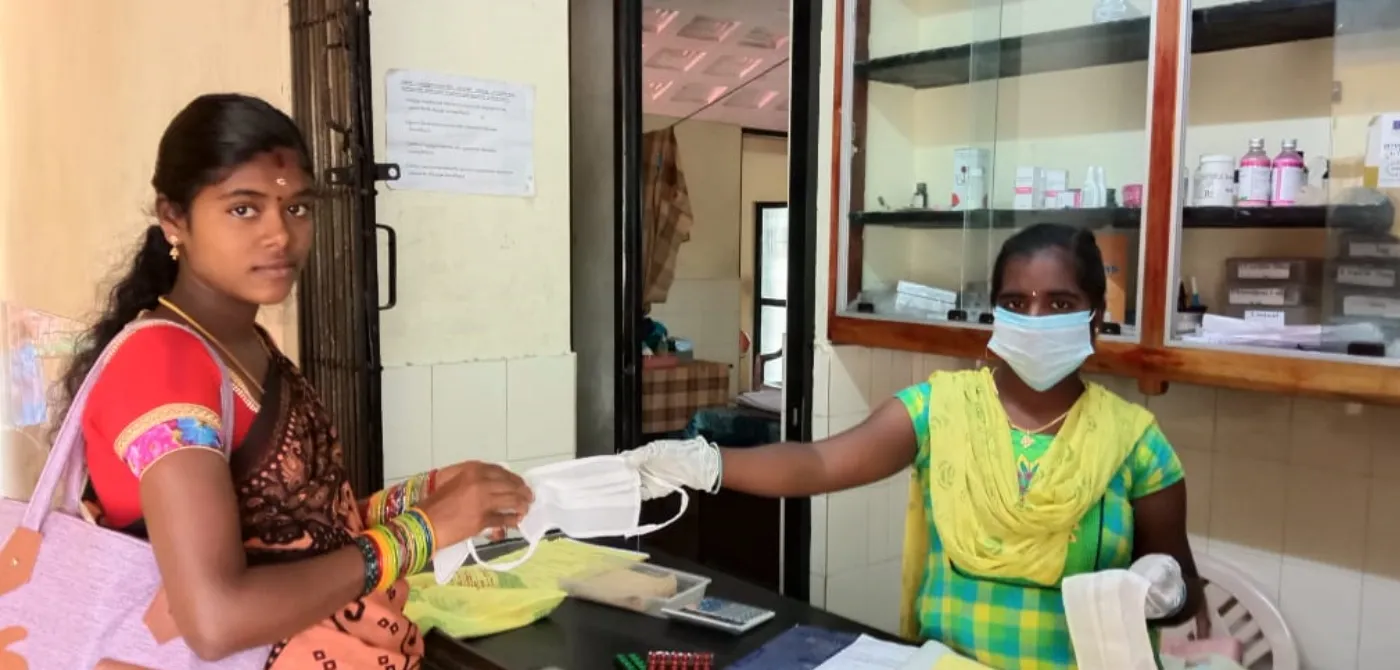
In this analysis, we draw on two studies carried out during 2020 and 2021 by the Rural Women’s Social Education Centre (RUWSEC), an organisation working in Chengalpattu district of Tamil Nadu, to describe how rural marginalised women’s lives were affected by the Covid-19 pandemic and the subsequent lockdowns, including the challenges they faced in accessing sexual and reproductive health services.
Tamil Nadu had the fourth highest number of Covid-positive cases in India during 2020-2022. Within the state, Chengalpattu district had the third highest number of confirmed Covid-19 cases and the second highest number of Covid-19 deaths.
The studies were intended to inform the RUWSEC’s response to the crisis in the villages where we worked. These studies, although limited in scope, provide important insights about the ways in which the pandemic exacerbated the challenges that women from marginalised communities routinely encountered and how their access to essential sexual and reproductive health services was affected.
Most of the women belonged to Dalit households and did not do any paid work. We spoke to women who had sought sexual and reproductive health services during the pandemic and to some frontline healthcare providers, including a gynaecologist running a private clinic.
Impact of Covid-19 on Women’s Lives
Livelihoods in crisis and intensified food insecurity: Almost all the respondents said that their households had no income during the pandemic because both men and women found it difficult to find work. Women, when desperate, were forced to work for meagre wages.
A 39-year-old Dalit woman with three adolescent children said,
During the second wave of Covid 19, agricultural work was available. But they allowed only four, five women at a time to work in the field. Although the wage was only Rs. 50, the women in our village fought with each other to get a chance to work. I worked three or four days a week. They gave Rs. 200 a day to a team of four women. I got my share of Rs. 50 and used the money for our food expenses. There were days when I got a wage of only Rs. 10 for two hours and we bought 200 ml of milk for that.
Managing household economic crises, particularly the family’s food needs, was primarily the responsibility of women during the Covid-19 lockdown. For some, it was difficult to even get one meal a day. A 21-year-old tribal woman with an infant recalled,
There was no job and no money on many days. Ours is a joint family and we did not eat for a few days. But two of my husband’s brothers were small school-going boys. They went and ate with the neighbours. We stayed hungry for many days during the pandemic.
The free supply of grains (mainly rice) through the public distribution system to poor households and the Covid-19 relief money of Rs. 4,000 given by the state government during the second wave provided a lifeline.
Increased stress and strained relationships: Women reported many instances of disagreement during the lockdown period because everyone was at home in a confined space for a long time. Added to this were the household economic and food crises, and the men turning to alcohol to cope with the stress. When the women argued with their husbands over this, they faced violence.
Men stretched to their limits sometimes attempted suicide. A woman who had been through much said,
During the pandemic, there was no income. We had difficulty repaying a loan. The person who gave the loan came to our house and quarrelled with us. When I questioned my husband, he drank poison. Luckily, my timely intervention saved him.
Exacerbation of intimate partner violence: According to the National Family Health Survey (NFHS-5) (2019-21), nearly 38% of ever-married women in Tamil Nadu had experienced spousal violence. A more recent study in the RUWSEC’s area of work also found that spousal relationships were rarely cordial—physical and sexual violence were regular events in women’s lives (Common Health 2021). The situation seems to have become worse during the pandemic because of its multiple stresses and crises.
For many women, non-consensual sex was a routine feature during the lockdown period.
With a few exceptions, women reported experiencing one or more forms of violence from their intimate partner or their in-laws during the pandemic. Many had faced serious physical and sexual violence, significantly affecting their sexual and reproductive health.

A 23-year-old woman who was born HIV positive and had married an HIV-negative person of her choice from another caste said,
My husband was fully drunk during the Corona time, beating me up badly. During the first lockdown, I was pregnant for the first time. He scolded me for getting pregnant and asked how we would proceed with the pregnancy without any money. He did not even allow me to switch on the fan. He did not let me eat food. He tortured me a lot. Maybe that is why I had a miscarriage. I was planning to postpone the next pregnancy, so I gave him condoms provided by the hospital (anti retroviral therapy centre) but he did not use them. Now I am pregnant a second time. The other day, he beat me badly on my head with a stick and it began to bleed.
For many women, non-consensual sex was a routine feature during the lockdown period. If they refused, it led to many problems in the family. Many women with adolescent children reported that their husbands compelled them to have sex. Even if the women refused, their husbands did not listen. This was a common complaint from all middle-aged women.
The absence of support systems during the lockdown made the situation more difficult. When women could not handle the violence they faced, they visited their natal home or sought external support from the RUWSEC’s community-based women’s protection committees, protection officers, or the police.
The restrictions on movement and the presence of the perpetrator at home at all times often cut off these sources of support. Two of the women we spoke to admitted to having attempted suicide because they could not cope with the violence.
Access to Health Services
Tamil Nadu has a good network of public health facilities, but during the second wave of Covid-19 all the public and private hospitals in the state were converted into Covid-19 care centres. Healthcare providers from primary health centres (PHCs) were diverted to hospital duty and nurses were charged with providing routine primary healthcare. Supply chains were disrupted and many routine services, including contraception, abortion, and pregnancy and delivery services, became unavailable or were restricted, especially at the lowest level.
Restrictions on mobility during the lockdowns and the limited availability of public transport facilities made access to higher level facilities difficult for many women from marginalised communities. Fear of contracting the Covid-19 infection in crowded district and medical college hospitals and household challenges such as the lack of income and intimate partner violence added to their difficulties.
Contraceptive services: Condoms were out of stock at local PHCs, resulting in unwanted pregnancies. A woman who thus got pregnant said,
My husband had been using condoms. As he works in a restaurant, he would come home once every three months and bring condoms. During the pandemic, he was at home all day. There was no supply of condoms in the nearby PHC and the private medical shop. So, he did not use one, and I conceived.
Public health facilities also temporarily stopped providing other methods of contraception. A nurse from a PHC said,
During the pandemic and lockdown, female sterilisation operations were not done at government district hospitals. Only a post-partum IUCD (intrauterine contraceptive device) was inserted when a woman went for a delivery. Others were told to come after the pandemic.
According to women, inserting IUCDs post-partum without informing them has been a routine practice in the public health facilities of the area. During the pandemic, women who had had an IUCD inserted without their knowledge faced difficulties because they had to make repeated visits to government hospitals or seek private medical care and pay for it at a time when money was hard to come by. A woman with a two-month-old baby said,
As I could not bear the pain and excessive bleeding, I visited a private doctor requesting her to remove the Copper T, and she did it. I paid Rs. 2,000 for the removal and she gave me medicines to improve my health. The cost of the drugs was Rs. 1,000.
Safe abortion services: Disruptions in the availability of contraceptive services led to many unwanted pregnancies. However, there were difficulties in obtaining safe abortion services. According to a PHC nurse,
On normal days in our PHC, medical abortion pills were provided up to eight weeks of gestation by the medical officer. For second-trimester abortion, we referred women to the general hospital. However, during the Covid time, we did not have medical abortion pills, and the service was also temporarily stopped in the general hospital because of a shortage of staff and doctors. All had been diverted to Covid screening and treatment.
Abortion services were reportedly available at the Chengalpattu Medical College hospital, but women feared going there because it was overflowing with Covid-19 patients. A woman who had an abortion said,
I went to a nearby PHC and asked for abortion pills and the nurse told me that they do not provide abortion services. She referred me to the government medical college hospital in Chengalpattu because the pregnancy had crossed eight weeks. But we were scared there would be many Corona patients in the Chengalpattu hospital. I already had two children and we could not manage a third. Finally, I went to a private hospital in Chengalpattu and had an abortion.
Those who terminated their pregnancy in the private sector paid a huge amount, which was beyond their means. The cost of an abortion ranged between Rs 12,000 and Rs. 30,000 depending on the type of facility, duration of stay, and a woman’s pre-existing health problems. Women mortgaged their jewels or borrowed money from neighbours and relatives to meet their abortion expenses in private hospitals. One of them said,
I had some gold jewellery and I mortgaged it to meet my abortion expenses. As I already have two children, I decided to take care of my health. We can earn money at any age but will not get our life back (referring to the risk of falling sick in the medical college hospital).
Pregnancy and delivery care: The women who were pregnant during the pandemic preferred to use their local PHC for antenatal care since it was close to their residence and accessible. However, a PHC staff nurse said that the PHCs did not do blood tests and ultrasonography tests for pregnant women during the pandemic but referred them to private facilities. The PHCs also advised pregnant women to have fewer check-ups to avoid exposure to the infection.
Further, the nurses or midwives conducted only normal deliveries in PHCs because the duty doctors were diverted to taluk and district hospitals for Covid-19 duty. Transportation to other hospitals was difficult during the pandemic. Some women reported that government ambulance services were unavailable for women in labour and they had to make other arrangements. Those who could not afford to do so had to settle for affordable, even if risky, modes of transportation. A woman said that she travelled on a two-wheeler despite her complications because she did not have the money for the taxi fare.
I went to a nearby PHC till the eighth month. They referred me to the government medical college hospital for the final month. There was no public transport, so we went to the general hospital with my husband on his bike. The nurse scolded me as my health was not good. But what could we do? If we took a taxi, we would have had to pay Rs. 2,000.
Access to medications for HIV: During the Covid-19 lockdown, primary and secondary-level government health facilities provided only limited services. A shortage of medicines for women living with HIV was reported for some months. Government hospitals were flooded with Covid-19 patients and an HIV-positive woman described the many problems she had in obtaining antiretroviral therapy from the district hospital.
Conclusions
The lives and livelihoods of women from marginalised communities in Chengalpattu district were severely affected by the Covid-19 pandemic. At the household level, poor rural women faced a severe financial crisis and had great difficulty in feeding their families. The lockdown confined people to their homes for a long period, leading to strained relationships among family members, especially husbands and wives.
Wife battering and abusive language were common while forced sex was widespread. But due to lockdown restrictions, women could not turn to their family members or other support systems. Sexual violations during the pandemic led to unwanted pregnancies and poor pregnancy outcomes because there were many challenges in accessing reproductive health services.
Though the national government announced that sexual and reproductive health services were essential services during the lockdown, the restrictions made it difficult to provide them. There was a disruption in the services regularly provided for maternal healthcare, safe abortions, and contraception.
Abortion services were unavailable at primary and secondary healthcare facilities. Women feared seeking abortion services at the Chengalpattu medical college hospital as it was overcrowded with Covid-19 patients. So they visited private hospitals and spent much more than they could afford at a difficult time.
There was a disruption in the services regularly provided for maternal healthcare, safe abortions, and contraception.
Poor women prefer to visit PHCs for pregnancy and delivery care services because they were close to their villages and easily accessible. However, the diversion of staff from PHCs during the pandemic meant that certain essential diagnostic tests and services were not available or only available sometimes. Government ambulance services were mainly used to transport Covid-19 patients and they were not available to take pregnant women to taluk and district hospitals.
Based on the study’s findings, it is evident that special care and attention should be paid while managing future pandemics, particularly in addressing the sexual and reproductive health issues of women from the marginalised sections. Second, creating a community-level support system for such women by involving local self-government leaders, self-help group women leaders, and frontline health workers is also necessary. Third, community-based organisations like the RUWSEC can help gather information about sexual rights violations and the healthcare needs of marginalised women. They could support the health and social sectors by reaching out to women in need with essential services.
Balasubramanian P. is the Executive Director of the Rural Women’s Social Education Centre (RUWSEC), an organisation working on the gender, sexual and reproductive health issues of marginalised people in Tamil Nadu.